Abstract
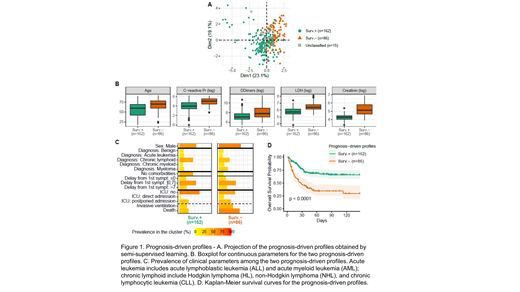
Background: The COVID-19 disease has spread throughout the world in an unprecedented way. France and Brazil confirmed the first cases in the European and South American regions with high incidence rates at the peak of the first wave of contamination along the year 2020. Patients with hematological disorders, especially malignancies, may be more vulnerable to SARS-CoV-2 infection because of the underlying disease and treatment. Since COVID-19 presentation is heterogeneous, from asymptomatic up to severe life-threatening forms and the patients with malignancies and COVID-19 admitted to the hospital show a wide range of clinical manifestations and laboratory abnormalities, it is still unclear for clinicians which patients, blood tests at admission and disease factors are associated with worse outcomes. Getting further insights into patients with specific diseases is of particular interest. We aimed to identify profiles of hematologic patients hospitalized with COVID-19 that would be associated with survival, and to assess the differences between cohorts. Methods: A binational cohort including all consecutive hematological patients aged 18 years or more with moderate or severe COVID-19, requiring hospitalization until December 2020 at two tertiary centers, from Paris, France and São Paulo, Brazil, was studied. Patients with a hospital stay of less than 24 hours were excluded. All patients were followed until the end of hospitalization; then, after discharge, survival data was recovered on medical charts or outpatient consultations, if data were available. Patient profiles were based on age, comorbidities, blood tests at admission, COVID-19 symptoms, and hematological disease characteristics. A semi-supervised learning method was first used to obtain the prognostic driven profiles; then, a classifier was identified to allow the classification of patients using only admission (baseline) data. Results: A total of 263 patients (135 from Brazil and 128 from France) were enrolled. Male patients (58.2%), elderly (≥ 65 years, 46%), with high comorbidities prevalence were frequent. Non-Hodgkin Lymphoma (29.3%), multiple myeloma (19.4%) and chronic myeloid disorders (12.9%) were the most frequent underlying hematological malignancies and 13.3% of patients had benign diseases. Most of the patients (59.7%) had undergone chemotherapy in the last six months before COVID-19 admission. The clinical presentation of COVID-19 was similar in the two countries. Fever (68.4%), dyspnea (60.1%) and cough (55.9%) were the main symptoms at admission. The ICU admission (56% versus 25%) and invasive ventilation (42% versus 19%) rates were notably higher among Brazilian patients due to scarce ICU beds during the peak of transmission in France. The overall in-hospital mortality rate was 115/263 (43.7% [95%CI 37.6-49.9]) and the median follow-up after admission was 63 days (IQR 40-98). There was no evidence of survival difference between countries after adjusting on age, comorbidities, and diagnosis. Two clusters were identified, segregating young patients with few comorbidities, low CRP, D-dimers, LDH and creatinine levels, with a 30-day survival of 77.1%, versus 46.7% in remainders. The profiles (clusters) were strongly associated with survival (p<0.001), even after adjusting on age (p<0.001) (Figure 1). We identified a set of rules to classify patients into the two profiles, using only information available at hospital admission, with a high accuracy rate (97.7% on the training set and 84.9% on the validation set). The baseline predictors consecutively selected by the model were the number of comorbidities, creatinine, CRP, a continuous regimen of chemotherapy, platelets and lymphocytes counts, a symptom of ageusia, dyspnea, hematological malignancy, high blood pressure, and symptom of myalgia. Conclusions: This analysis allowed to identify two profiles of hospitalized hematological patients with COVID-19 that have a different outcome when infected with SARS-CoV-2. The results showed the importance of CRP, LHD, and creatinine in COVID-19 presentation and prognosis, whatever the geographic origin of the patients. The identification of patterns and clinical manifestations experienced by hematological patients during moderate or severe SARS-CoV-2 infection might be helpful to medical staff in the care management and in the allocation of scarce resources.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal